An Everyday DNA blog article
Written by: Sarah Sharman, PhD, Science writer
Illustrated by: Cathleen Shaw

If you have been out and about this month, you may have seen teal flags, bows or banners in your neighborhood or around town. Teal is the color that is designated for ovarian cancer survivors, patients, and their supporters. Although many national cancer organizations have long recognized September as Ovarian Cancer Awareness Month, this year President Biden officially declared September 2021 as National Ovarian Cancer Awareness Month.
The official recognition of an awareness month is important for raising funds to support research and technology used to detect, treat, and eliminate ovarian cancer. Let’s learn about ovarian cancer and what scientists are doing to develop new ways to detect ovarian cancer earlier and improve treatment strategies.
What is ovarian cancer?
Cancer is a disease in which some of the body’s cells grow out of control, and in many cases spread throughout the body. Normally, cells grow and multiply to form new cells to replace old or damaged cells. In cancer, the orderly process of replacing cells breaks down, and abnormal or damaged cells grow and multiply instead of dying and being replaced.
Ovarian cancer originates in cells of the ovaries, fallopian tubes, or peritoneum, which is the tissue that lines the abdominal wall and covers the abdominal organs. Ovaries are the reproductive organs that produce eggs in females. They are also the main source of the female hormones estrogen and progesterone.
The ovaries are made up of three types of cells that can each develop into a different type of tumor. Epithelial tumors originate from the cells that line or cover the outer surface of the ovaries and fallopian tubes. The majority of ovarian tumors are epithelial in nature, accounting for 85 to 90 percent of malignant ovarian tumors. Germ cell tumors start from the cells that produce the eggs, while stromal tumors begin in the structural tissue cells that hold the ovary together and produce female hormones.
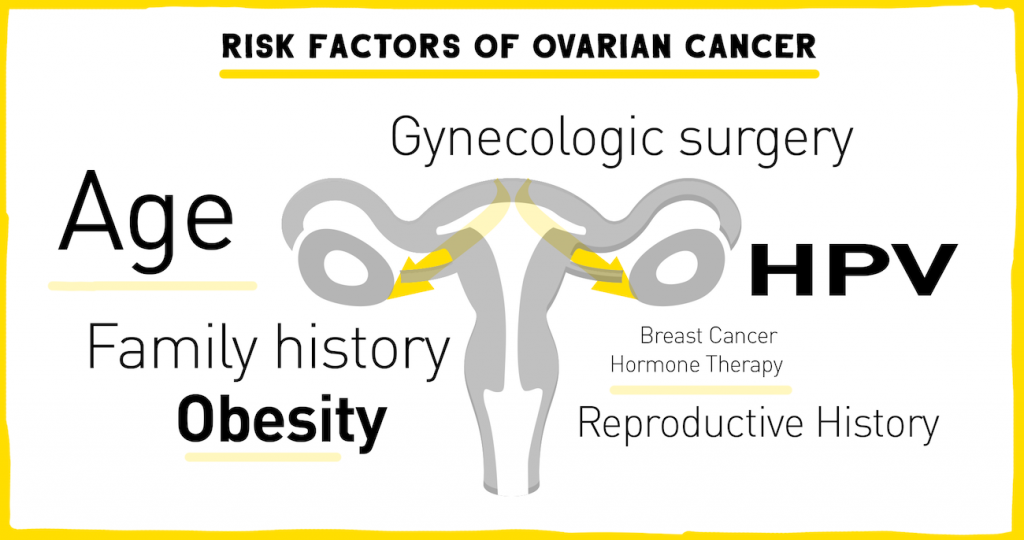 The risk of a woman being diagnosed with ovarian cancer in her lifetime is 1 in 78. Researchers have discovered several risk factors that might increase a woman’s chance of developing epithelial ovarian cancer. Age and family history of ovarian cancer are currently the two strongest risk factors. Ovarian cancer is rare in women under the age of 40 with half of all ovarian cancers being found in postmenopausal women 63 years of age or older.
The risk of a woman being diagnosed with ovarian cancer in her lifetime is 1 in 78. Researchers have discovered several risk factors that might increase a woman’s chance of developing epithelial ovarian cancer. Age and family history of ovarian cancer are currently the two strongest risk factors. Ovarian cancer is rare in women under the age of 40 with half of all ovarian cancers being found in postmenopausal women 63 years of age or older.
About one in ten women who are diagnosed with ovarian cancer will have either a strong family history of ovarian cancer or a mutation in a gene that increases risk of the disease. A small portion of ovarian cancers occur in women with inherited mutations in the BRCA1/BRCA2 genes, as well as a number of genes related to other family cancer syndromes linked to an increased risk of ovarian cancer (PTEN, STK11, MUTYH, and many genes that cause hereditary nonpolyposis colon cancer).
In addition to inherited mutations that increase risk for being diagnosed with ovarian cancer, all ovarian cancer cells acquire mutations as the tumor cells divide and grow. Scientists have not yet specifically linked any environmental or lifestyle factor to the cause of acquired mutations in ovarian cancer. Although it is still rare to get ovarian cancer, the risk factors above, along with obesity, gynecologic surgery, HPV infection, breast cancer, hormone therapy, and never becoming pregnant, are all thought to increase a woman’s chance of developing ovarian cancer.
How is ovarian cancer diagnosed and treated?
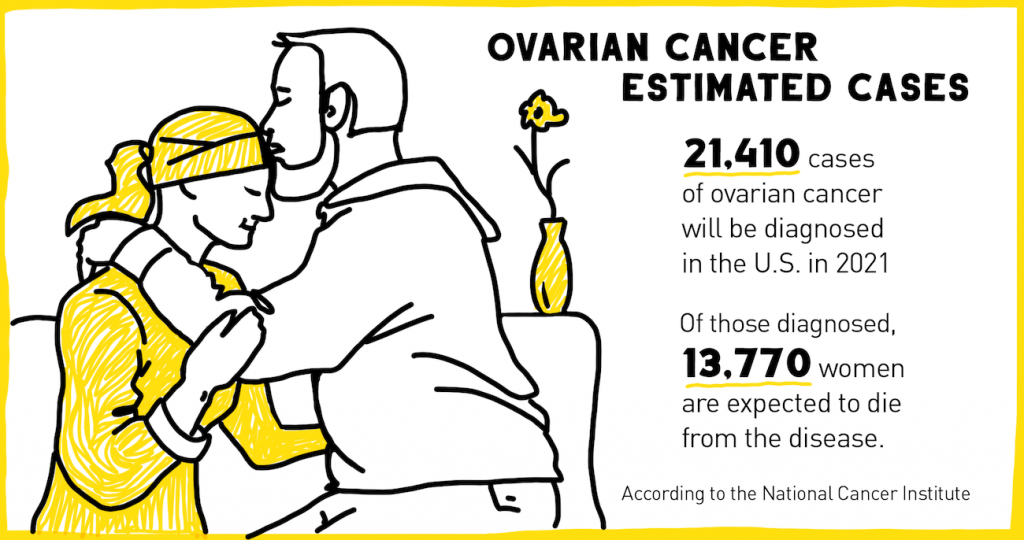
According to the National Cancer Institute, an estimated 21,410 cases of ovarian cancer will be diagnosed in the United States in 2021. Of those diagnosed, 13,770 women are expected to die from the disease. A major factor for the high mortality rate of ovarian cancer is the lack of early diagnostic tests.
 Unlike breast cancer where mammograms can detect very early signs of cancer, screening for ovarian cancer is difficult. In addition, early ovarian cancer often has no symptoms, and the few symptoms that do occur are associated with other disorders. As a result, ovarian cancers often go undetected until they have reached advanced stages. Pelvic ultrasound and blood tests for high levels of a protein called CA-125 that is common in ovarian cancer are currently the best tests for diagnosing ovarian cancer.
Unlike breast cancer where mammograms can detect very early signs of cancer, screening for ovarian cancer is difficult. In addition, early ovarian cancer often has no symptoms, and the few symptoms that do occur are associated with other disorders. As a result, ovarian cancers often go undetected until they have reached advanced stages. Pelvic ultrasound and blood tests for high levels of a protein called CA-125 that is common in ovarian cancer are currently the best tests for diagnosing ovarian cancer.
Ovarian cancer patients generally have surgery to remove as much of the tumor as possible, which sometimes involves removing the ovaries, fallopian tubes, or uterus. Surgery is usually combined with chemotherapy to stop the growth of cancer cells by killing the cells or by stopping them from dividing. Immunotherapy, which uses the patient’s own immune system to fight cancer, is in clinical trials for use in ovarian cancer. Targeted therapies that identify and attack specific cancer cells are also used in ovarian cancer treatment. For example, drugs called PARP inhibitors can be administered to women whose tumor has mutations in BRCA1/2.
The five-year survival rate is over 90 percent when ovarian cancer is diagnosed and treated at its earliest stage. However, as mentioned above, because of the lack of reliable screening tests only 20 percent of cases are found early. If the cancer is found in a late stage, the five-year survival rate can be as low as 28 percent.
What are scientists doing to improve treatment strategies?
While progress has been made in the field of ovarian cancer, not all treatments are effective for all patients. In addition, treatments that initially work well for a patient can become ineffective over time as the tumors become resistant to the drug. There is much research ongoing in the field to identify new drugs, new drug targets, and new combinations of drugs to overcome current treatment limitations.
 HudsonAlpha Institute for Biotechnology Faculty Investigator Sara Cooper, PhD, is focused on understanding the differences between tumors and how resistance develops so that doctors can more accurately determine the right treatment for the right patient at the right time in their treatment. Cooper’s lab is using genome-wide CRISPR screening methods to identify genes associated with chemotherapy resistance in ovarian cancer. This information can be used to make predictions about how a patient might respond to each possible treatment.
HudsonAlpha Institute for Biotechnology Faculty Investigator Sara Cooper, PhD, is focused on understanding the differences between tumors and how resistance develops so that doctors can more accurately determine the right treatment for the right patient at the right time in their treatment. Cooper’s lab is using genome-wide CRISPR screening methods to identify genes associated with chemotherapy resistance in ovarian cancer. This information can be used to make predictions about how a patient might respond to each possible treatment.
The team hopes to use this information to build tools that give physicians the ability to predict what a patient’s response to treatment will be. This will help them avoid administering a treatment that will not work, and allow them to administer a treatment that is most likely effective.
Cooper and her longtime collaborator Rebecca Arend, MD, an assistant professor in the University of Alabama at Birmingham (UAB) Division of Gynecologic Oncology and associate scientist in the Experimental Therapeutics Program at the UAB Comprehensive Cancer Center, are also studying new treatments for ovarian cancers with resistance to platinum-based chemotherapies. In a recent study, the team tested a new drug that inhibits a signaling pathway that is associated with a poor prognosis in ovarian cancer.
Their data showed that a combination of the inhibitor and a chemotherapy drug called paclitaxel enhances the immune system and decreases tumor growth better than either agent alone. These data, generated using a mouse model of ovarian cancer, have motivated further investigation of this pathway in human tumors. Those studies have revealed evidence supporting the potential for this strategy in patients with ovarian cancer.
These are just two examples of how scientists and physicians are trying to find new drugs or treatment strategies to overcome chemotherapy resistance and more successfully treat ovarian cancer.