An Everyday DNA blog article
Written by: Sarah Sharman, PhD, Science writer
Illustrated by: Cathleen Shaw
Cancer. Just reading the word invokes a lot of emotions in many people. Fear. Anger. Sadness. Confusion. Numbness. Anxiety. Uncertainty. Guilt. Empathy. Whether you have a personal connection to cancer or not, we are all aware of the devastating nature of the disease. In the United States alone, an estimated 1,806,590 new cases of cancer were diagnosed in 2020. Of these cases, breast cancer was the most frequently diagnosed (although lung cancer was a close second).
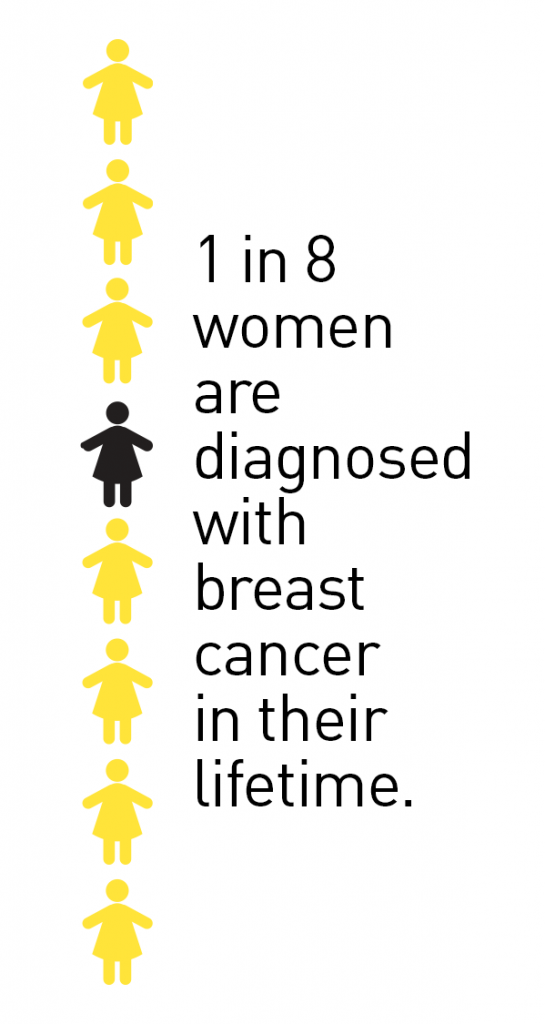
One in eight women in the United States will be diagnosed with breast cancer in her lifetime. While this number is still high, the breast cancer death rate has been declining since the early 2000s. Several factors like improved detection screening and the application of more personalized treatments have contributed to the decreased death rate. Let’s learn how the application of genomics to breast cancer research has helped spark many breakthroughs in both early detection and treatment of breast cancer.
Breast cancer: facts, causes and risk factors
Breast cancer is a disease in which cancerous cells form in the tissues of the breast. In breast cancer, damaged or abnormal breast cells that would normally die and be replaced by new cells are allowed to grow and continue multiplying. This buildup of cells can form a mass of tissue called a tumor.
The exact cause of most breast cancers is unknown. However, scientists and physicians believe that breast cancer is caused by damage to a cell’s DNA. The damaged DNA often gives the cell a survival or growth advantage, allowing it to live on and multiply when it should not. Why and how the DNA becomes damaged is unknown but genetic and environmental factors, or a combination of both, are thought to play a major role.
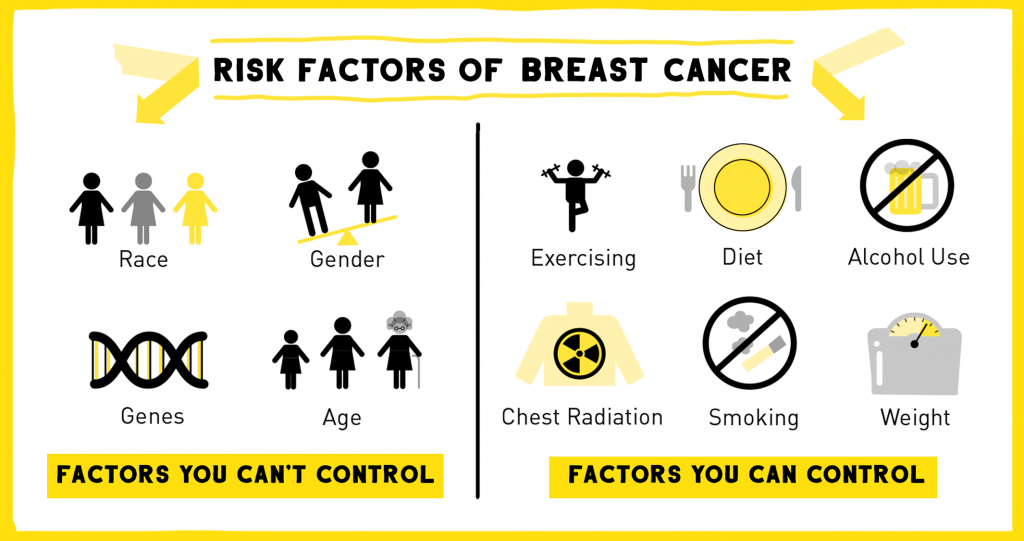
Scientists have determined several risk factors that may increase a person’s chance of getting the disease. Many environmental and lifestyle risk factors can be controlled or modified. Avoiding a sedentary lifestyle by getting ample exercise, eating a nutritious and well-balanced diet, drinking alcohol only in moderation, avoiding radiation to the chest, and limiting combined hormone replacement therapy can all reduce the risk of breast cancer.
Other risk factors are part of your very genetic makeup and cannot be changed. These include being born female (women are 100 times more likely than men to get breast cancer), aging (most breast cancers are found in women aged 55 and older), and inheriting certain gene changes (5-10 percent of breast cancers are thought to be hereditary).
Having one or more of these risk factors does not mean that you will be diagnosed with breast cancer. In fact, 60-70 percent of people with breast cancer have no connection to risk factors at all, and other people with risk factors will never develop cancer. Being vigilant with annual mammograms and performing regular breast self-exams are important in the early detection of breast cancer for all women regardless of their risk category. Mammograms are the only breast cancer screen that have been proven to reduce breast cancer deaths.
How are genetics helping breast cancer treatment?
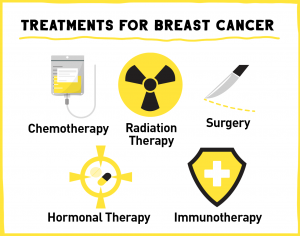 Breast cancer treatment is continually being improved as the scientific and medical communities learn more about the disease. Currently, treatment options include various combinations of surgery, radiation, chemotherapy, hormonal therapy, and immunotherapy, tailored to each individual’s specific type and stage of cancer.
Breast cancer treatment is continually being improved as the scientific and medical communities learn more about the disease. Currently, treatment options include various combinations of surgery, radiation, chemotherapy, hormonal therapy, and immunotherapy, tailored to each individual’s specific type and stage of cancer.
By studying the genetic makeup of a patient’s tumor, physicians can often make more informed treatment decisions. For example, in breast cancer some of the body’s hormones and other molecules can accelerate tumor growth by binding to receptors on the tumor cell’s surface. The molecules bind the receptor like a key in a lock and give the cell energy to grow and multiply. In some tumors, faulty genes provide instructions to make too much or too little of a receptor or its binding partner. Hormonal therapy and immunotherapy both target specific receptors on the cancer cells to block the receptors and restrict the tumor’s growth.
All breast cancers are tested for changes in three genes that instruct the body to make estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). The presence or absence of one or all of these receptors helps to direct the treatment plan. ER-positive and PR-positive breast cancers can be treated with hormone therapy. HER2-positive breast cancers are treated with targeted therapies like the monoclonal antibody trastuzumab that blocks the HER2 receptor and helps shrink the tumor. These are just a few examples of how genetic profiling of tumors can help physicians put together the best treatment plan for each individual patient.
Can elective genetic testing improve breast cancer surveillance?
In addition to informing treatment decisions, genetics is also being applied to breast cancer screening. Using the rapidly increasing amount of genetic data, scientists are finding many more associations between genetic changes and breast cancer risk. In total, more than a dozen breast cancer predisposition genes have been defined. Most of the gene mutations also increase the risk of other cancers.
Mutations in two genes, called breast cancer gene one (BRCA1) and breast cancer gene two (BRCA2), carry the highest risk of developing breast cancer. A gene called partner and localizer of BRCA2 (PALB2) has emerged as another important genetic risk factor for breast cancer. It is estimated that 35 percent of women with a mutated PALB2 gene will develop breast cancer by the age of 70.
Currently, experts only recommend BRCA1/2 or expanded panel genetic testing for certain people with an increased risk of having an inherited genetic mutation related to breast cancer. Increased risk categories include women having a family member with a known inherited genetic mutation associated with breast cancer, and women with a personal or family history of breast cancer or ovarian cancer at age 45 or younger.
 A genetic testing initiative in North Alabama provides compelling evidence that widespread genetic testing could be beneficial for the detection of mutations in genes that increase risk for breast cancer and other heritable cancers. Over the past six years, a program from HudsonAlpha Institute for Biotechnology (led by faculty researcher Sara Cooper, PhD) and Kailos Genetics has offered free or reduced cost genetic tests to residents of five North Alabama counties through the Information is Power initiative. The test looks at several dozen genes associated with increased risk for breast, ovarian, colon, and endometrial cancers.
A genetic testing initiative in North Alabama provides compelling evidence that widespread genetic testing could be beneficial for the detection of mutations in genes that increase risk for breast cancer and other heritable cancers. Over the past six years, a program from HudsonAlpha Institute for Biotechnology (led by faculty researcher Sara Cooper, PhD) and Kailos Genetics has offered free or reduced cost genetic tests to residents of five North Alabama counties through the Information is Power initiative. The test looks at several dozen genes associated with increased risk for breast, ovarian, colon, and endometrial cancers.
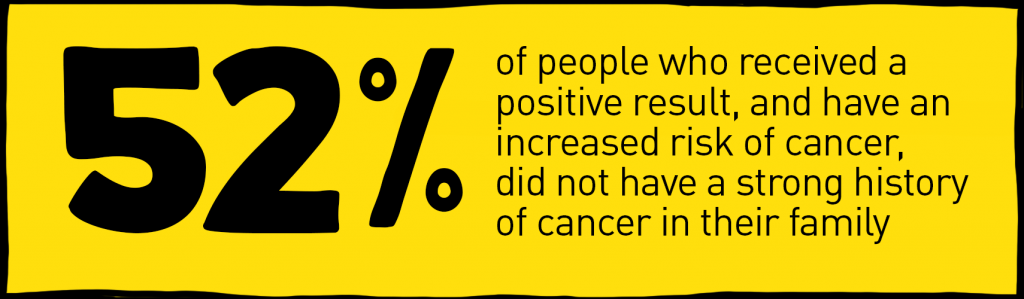
As of September 2021, more than 5,200 people have been part of the initiative. Of these, 4.37 percent of participants received a positive result and have an increased risk of cancer. Surprisingly, 52 percent of people who received a positive result did not have a strong family history of cancer, meaning it is likely they would not have been offered a genetic test at their physician’s office. While the number of people receiving positive results is relatively small, the information they receive puts these individuals on a path to proper screening, early detection, and sometimes even the possibility of preventing cancer altogether. As the cost of genetic testing has declined, this program shows the benefits elective genomic testing could provide to help individuals make more informed health and disease screening decisions in their futures.
The Information is Power initiative continues its efforts to offer testing in the Alabama community with an emphasis on making this program accessible to all. With support from local and regional granting agencies, the initiative is currently expanding its reach into additional counties in Alabama, with the hopes to provide inexpensive, elective testing of increased cancer risk to more people across the state.