Although the human brain weighs only three pounds, it is arguably one of the most complex and hard-working organs in the human body. It controls thought, memory, emotion, touch, motor skills, vision, breathing, temperature, hunger, and every process that regulates our body. When the brain is healthy, it functions quickly and automatically. But the results can be devastating when something goes awry.
Neurodegenerative diseases are a class of devastating diseases in which cells of the brain and nervous system stop functioning correctly and eventually die. Scientists discovered several hundred types of neurodegenerative diseases that collectively affect millions of people worldwide.
For centuries, scientists marveled at the brain in health and disease states. Over the past few decades, scientists understand the brain and the nervous system more clearly. Listen to Tiny Expeditions Season 3, Episode 3, “When our brains fail us: an exploration of neurodegenerative diseases,” to journey into the brain and learn how scientists unravel the genetics behind many neurodegenerative diseases to help develop better diagnostic and treatment options.
Behind the scenes
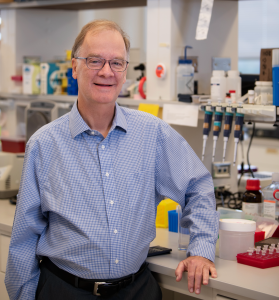 Huntingtin (HTT) was the first disease-associated gene to be molecularly mapped to a human chromosome. The same genetic discovery also led Rick Myers, PhD, (left) down his career path of discovering the genetic cause of various neurodegenerative diseases. Over the past decade, Myers and his lab contributed to countless neurodegenerative and neuropsychiatric disease discoveries. They study complex nervous system diseases, including Huntington’s disease, Alzheimer’s disease, frontal temporal dementia (FTD), bipolar disorder, schizophrenia, and amyotrophic lateral sclerosis (ALS).
Huntingtin (HTT) was the first disease-associated gene to be molecularly mapped to a human chromosome. The same genetic discovery also led Rick Myers, PhD, (left) down his career path of discovering the genetic cause of various neurodegenerative diseases. Over the past decade, Myers and his lab contributed to countless neurodegenerative and neuropsychiatric disease discoveries. They study complex nervous system diseases, including Huntington’s disease, Alzheimer’s disease, frontal temporal dementia (FTD), bipolar disorder, schizophrenia, and amyotrophic lateral sclerosis (ALS).
One of their current goals is to develop predictive blood-based diagnostic tests that can detect neurodegenerative diseases earlier than current diagnostics. Myers’ lab previously discovered circulating biomarkers of early colon lesions called colorectal adenoma that could eventually develop into colon cancer. The biomarkers were DNA or RNA molecules released into the blood by cells in response to cell damage, stress, or death.
As Dr. Myers mentioned in this episode, the lab made great progress in finding biomarkers for Alzheimer’s disease. Stay tuned in the coming months because Dr. Myers’ lab is pushing the forefront of biomarker detection. To learn more about biomarkers and their use in the diagnostic and clinical trials fields, read this Everyday DNA blog post.
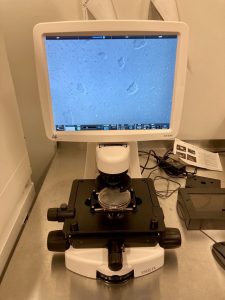
 A major challenge in neurological disease research that Dr. Myers and his lab are addressing is the difficulty of gaining access to samples from developing brains. We were excited to take a trip to the Myers lab and meet up with senior scientist Lindsay Rizzardi, PhD (left) to learn more about inducible pluripotent stem cell (IPSC) technology. Pictured below are the cells we looked at during our lab tour.
A major challenge in neurological disease research that Dr. Myers and his lab are addressing is the difficulty of gaining access to samples from developing brains. We were excited to take a trip to the Myers lab and meet up with senior scientist Lindsay Rizzardi, PhD (left) to learn more about inducible pluripotent stem cell (IPSC) technology. Pictured below are the cells we looked at during our lab tour.
As we learned in the lab, IPSCs are stem cells that come from a person’s skin that have been manipulated to go back into a stem-cell-like state. The cells can then be manipulated further and turned into neurons that are growing in a dish. Once they are in this state growing in a dish, researchers can perform experiments on them. These cells help Myers’ lab transfer data gleaned from experimental models into human beings.
Another cutting-edge technology that we briefly heard about in the lab tour is single-cell analysis. Historically, brain samples included all the cell types of the brain mixed together. This means that if only one subtype of brain cell is involved in the disease pathology, its signal could be covered up by more abundant cell types. The single-cell analysis allows Dr. Myers and his team to study neurodegenerative diseases on a more granular cell-by-cell basis. Looking at individual cells provides scientists with more precise information on the genetic differences between the brain of someone with a disease and the brain of someone without the disease.

Nick Cochran, PhD (pictured left) focuses his research on using genomic approaches to diagnose and treat Alzheimer’s disease and related dementias. Dr. Cochran and his lab collaborate with many other research institutes worldwide to compile large data sets of patients with and without neurodegenerative diseases to identify new genes or genetic variants that are associated with disease onset and progression.
(pictured left) focuses his research on using genomic approaches to diagnose and treat Alzheimer’s disease and related dementias. Dr. Cochran and his lab collaborate with many other research institutes worldwide to compile large data sets of patients with and without neurodegenerative diseases to identify new genes or genetic variants that are associated with disease onset and progression.
Dr. Cochran described one of those collaborative projects to us during the episode. The official name of the collaboration is Multi-Partner Consortium to Expand Dementia Research in Latin America (ReDLat). ReDLat was launched to expand dementia research in Latin America. There is a high burden of various dementias in South America, and much of the current dementia research does not include a representative Latin American population. Dr. Cochran and other consortium members are looking to right-size genetic association studies for underrepresented populations.
The consortium aims to identify the unique genetic and socioeconomic determinants of health that drive Alzheimer’s diseases and other dementias in Latin America. Scientists involved in the project are using neuroimaging, genetic, and behavioral data on over 4,000 individuals from Argentina, Brazil, Chile, Colombia, Mexico, Peru, and the United States to offer a unique understanding of the genetic and environmental underpinnings of dementia.
Sarah Sharman 00:00
Season Three of Tiny Expeditions is made possible through the support of our sponsor EBSCO Information Services, the leading provider of online research content, search technologies, and workflow tools, serving public libraries, schools, academic institutions, corporations, and medical institutions around the world, proudly delivering information access for researchers at all levels. Find them online at ebsco.com. That’s EBSCO.com.
Rick Myers 00:35
It’s just fascinating that you have this incredibly complex, wonderful organ, that one spelling mistake ends up causing it to eventually degrade and die and cause the individual to die. And can we understand that? And then can we do something about it?
Chris Powell 00:58
Welcome to Season Three, episode three of Tiny Expeditions. Today’s episode is an interesting one. We are going to use our brains to talk about brains.
Sarah Sharman 01:10
Actually, Chris, we’re talking about what happens when things go wrong with the brain. We’re talking about neurodegenerative diseases. I’m Dr. Sarah Sharman, and I’ll help us walk through the science.
Chris Powell 01:20
And I’m Chris Powell. I’m going to be our storytelling guide for today.
Sarah Sharman 01:23
Today you will hear from two Hudson Alpha faculty members. And you’ll take the journey into the lab with a senior scientist.
Chris Powell 01:30
So, let’s get started. Let’s dive into the world of neurodegenerative diseases.
Rick Myers 01:36
I’m Rick Myers.
Sarah Sharman 01:38
Rick is a man of many titles here at HudsonAlpha. He is the Chief Scientific Officer, President Emeritus, M. A. Loya Chair in Genomics, and a faculty investigator.
Chris Powell 01:49
And for those of you who remember the Human Genome Project, the groundbreaking project that really gave birth to all of this well, Rick and his lab at Stanford were a part of that project as well.
Rick Myers 02:00
I’m a human geneticist and genomicist. I work on how genes affect humans and really other organisms as well.
Sarah Sharman 02:08
You’ve probably all heard of diseases like ALS, Alzheimer’s, and Huntington’s disease, but maybe the term neurodegenerative disease is less familiar to you. It turns out these are all diseases under this umbrella category.
Rick Myers 02:21
When something is called a neurodegenerative disease, this means that something goes wrong with neurons, and they die. And that can be in the brain or in the spinal cord or in the peripheral nervous system as well. Neurons are key cells that have very specific kinds of properties that are different from most other cells. They fire electrical signals that have to do with how our nervous system works. And when neurons start to die, because they are connected to many other neurons and other cells, then that can affect how these downstream neurons live or then eventually die. So eventually, you may get cell death all over the brain for a disease that starts in the center of the brain, like Huntington’s disease or Parkinson’s disease.
Chris Powell 03:12
The list of diseases we’re talking about today, ALS, Alzheimer’s, Huntington’s, these are names that we know in large part because most of us are affected by these diseases. We either know someone or have a family member, or maybe we ourselves have been diagnosed with them. We are keenly aware of how insidious these diseases are. And they impact such a large portion of our population.
Rick Myers 03:36
One of the striking things is that the world has identified about 600 different neurodegenerative diseases. Most of those are really, really rare, you would have never heard on them. They affect relatively small numbers of people, I mean, maybe even dozens that have been identified or low, hundreds identified around the world. And they range from those rare diseases to Huntington’s disease, which has 30,000 to 40,000 people with the disease in the United States with a lot more, maybe twice that number at risk. And then Alzheimer’s has almost 6 million people in the United States with Alzheimer’s disease. And that number is increasing as our population ages, and then worldwide, that’s in the many tens of millions of people with the most common neurodegenerative disease, Alzheimer’s disease.
Nick Cochran 04:26
And those are just the people who are living with these diseases.
Sarah Sharman 04:30
And that’s Dr. Nick Cochran, faculty investigator at HudsonAlpha.
Nick Cochran 04:34
You have to think about the ripple effect that this has on family caregivers and things like this. So, this is one thing we’ve been trying to capture more recently in statistics is the economic impact this can have not only on the people directly affected by disease and those direct health care costs, but the unpaid time that family members have to put in, but you know, is also an economic impact of these diseases.
Chris Powell 05:01
We see how impactful these diseases are. So, where do we even begin trying to study them?
Rick Myers 05:07
So, it’s interesting, if you’re gonna want to understand the disease, it really helps to understand what causes it. And in some, and maybe even many of these, clearly genetics plays a role. There is simple genetics in the sense of Huntington’s disease because there’s one gene with one spelling mistake, one mutation. And if you get that mutation, you will get the disease if you live into your mid to late 30s, or longer. It’s an all or none thing.
Let’s take Alzheimer’s disease as another example. We now know that there are about seven to ten genes, that if you have a mutation, a spelling mistake, in one of those genes, you will get Alzheimer’s disease. The problem is those seven to ten genes account for less than 1% of all Alzheimer’s disease, most of it, we still don’t know the causes of Alzheimer’s, or we know that it’s a combination of multiple genes, some of which we might know.
Sarah Sharman 06:08
We’ve talked a lot in previous episodes about how changes in the genetic code itself can cause diseases in plants, animals, and humans. It turns out that diseases can also be caused by changes in how genes are regulated or turned on and off.
Nick Cochran 06:22
Gene regulation is all about how much or how little of a protein a cell produces. There are areas of DNA that are involved in gene regulation. And we use all sorts of different approaches to understand it. And understanding it at a super-fine level of detail is something that not a lot of people are doing. If we can gain that information, we can understand whether genetic variation within those regions of DNA that are important for gene regulation may give risk for a certain disease. And that goes back to that first point that I was making, that maybe if we can find those key types of genetic variation, we can get those individuals enrolled and either research or clinical studies.
Rick Myers 07:08
Another area that our laboratory works on is trying to understand the neurons themselves, human neurons, the cells by themselves, not inside a person. It’s really hard to study neurons in a living person. Can we look at those neurons, either in post-mortem brain tissue or in this new technology that allows us to actually grow human neurons starting from skin cells from people? These are called iPS cells that you can then differentiate into neurons.
Chris Powell 07:45
This new technology definitely piqued the interest of both myself and Sarah. So, we wanted to see for ourselves what this looked like. We met up with Dr. Lindsay Rizzardi in Dr. Myers’ lab.
Sarah Sharman 07:58
Hey, Lindsay.
Lindsay Rizzardi 08:00
Hey!
Chris Powell 08:00
So you’re Lindsay?
Lindsay Rizzardi 08:01
I am! Welcome to the tissue culture room.
Chris Powell 08:04
Thanks for letting us come in.
Lindsay Rizzardi 08:05
Yeah, anytime you guys want to check out some IPSC Yes, definitely. Awesome.
Chris Powell 08:11
Oh, you’ve got it up here ready?
Lindsay Rizzardi 08:12
I do. I was just checking these guys. So, these are induced pluripotent stem cells that we’ve been growing in the lab. And these guys are about ready to get split for differentiation. You can see them here. They like to grow in these little clumps because there’s a lot of important signaling that happens between these cells as they’re growing. And they really don’t like to be on their own, they’ll try to find their buddies. But when we get ready to differentiate them, we have to split them into the single cells so that then they can respond to the growth factors or the genes that we’ve turned on in these cells to differentiate into the cell types that we’re interested in.
Sarah Sharman 08:55
So, what do these cells start out as?
Lindsay Rizzardi 08:58
So they were initially grown from human fibroblasts. You can get these from skin punches that people do for normal medical procedures that they may need. And then they get reprogrammed back into this IPSC state, which is why it’s called an induced pluripotent stem cell state because you take these fibroblasts and induce them to revert back to a pluripotent state. And so you can do that by a cocktail of transcription factors activating them, and this basically wipes the epigenetic landscape clean, and you start fresh. And now you can have this potential to differentiate into whatever cell type that you might be interested in.
Chris Powell 09:33
So we’re literally changing the cell or the function of the cell?
Lindsay Rizzardi 09:37
Yeah, exactly right. And then we can redirect that cell to have whatever phenotype that we want as far as being a neuron or a cardiac cell or microglia as long as we know which factors they need to go down that differentiation pathway.
Sarah Sharman 09:58
So, what are you using them for?
Lindsay Rizzardi 10:01
So for these particular cells, we can induce the expression of a gene that will turn the cells into neurons. And so then what we plan to do with these neurons is a lot of functional genomics assays. And the assays that we tend to run are called CRISPR inhibition screens, because our lab is really interested in understanding the regulatory parts of the genome that control gene regulation. And so with CRISPR inhibition, what we have is a Cas9 enzyme that no longer cuts DNA, but it can bind very specifically to certain sites in the genome based on what guide RNAs we give it. And then we’ve attached it to a repressive domain, that when you land this at a particular region of the genome, it’ll repress that region so it can’t function anymore. And then that way, we can see what the effects are on gene expression because for many regulatory regions of the genome, we don’t know what the target gene is.
And so by doing this in a large genome-wide screening scale, we can figure out for each part of the genome, when you inhibit it, what genes are changing that expression, and that way, we can identify these links between this piece of DNA regulate to this gene. And that’s really important for what we’re interested in, which is studying neurodegenerative diseases, as well as other neurological disorders. Because we know some of the genes that are affected in these diseases, but we don’t always know how they’re regulated and how this regulation goes awry. So, this is a really good way to do this. And with single-cell technologies we are able to do this, you know, kind of in large cell numbers and assaying large parts of the genome at once.
Chris Powell 11:35
So we go from here to single cell analysis.
Lindsay Rizzardi 11:38
That’s right. So we take these cells once we’ve differentiated them. And then, we’ve added our CRISPR system and added our guide RNAs that target each region of the genome. Each cell will get one guide RNA, and target one region of the genome. And so together, if we assay 100,000 cells, we’re assaying 100,000 regions of the genome at once. And so we can look at the effects of that on transcription, which is going to be that gene expression change that we’re looking for. And in a single cell, we can say, Okay, this cell got this guide RNA, which inhibits region A, and genes, you know, XY and Z changed expression. So they must be the ones being regulated by this piece of the genome. So it’s really cool. Yeah, and we’re doing this not only with neurons, but also microglia as well. So for IPSC is, you know, the world is your oyster as far as what you can turn them into and what pathways you can study as long as you know the right cocktail of either transcription factors that you need to differentiate them into that cell type, or the combination of reagents and growth factors that you might need to add to the media to induce them to grow into that particular cell type.
Sarah Sharman 12:48
Many of these diseases are so devastating and ultimately fatal because they are not detected until the individual begins showing symptoms. By the time symptoms show up in some of these diseases, irreversible damage has already been done to the brain. A diagnostic tool called blood-based biomarkers have begun to show promise for the early detection of diseases like cancer. A small sample of an individual’s blood is analyzed for what we call biomarkers which can be certain proteins or nucleic acids in the blood. These biomarkers have the potential to be applied to many aspects of neurodegenerative disease research.
Rick Myers 13:24
The new drugs have not worked probably because they are starting to treat too late. So, what if we could detect early, even pre symptomatically before you have any symptoms? So, my lab has specialized partly in seeing if we can develop blood tests, take a little bit of blood, and then look to see if there’s something floating around in the bloodstream that’s indicative of Alzheimer’s disease, or Huntington disease or some other disease, for instance. So, we’ve been able to do this as a least preliminary test and Alzheimer’s disease. And while it’s not ready for clinical use, we sure enough, we have found biomarkers. These are in the form of in our case of specific small RNA, something called micro RNAs and other small RNAs. And we see those floating around in the bloodstream of people with Alzheimer’s disease, but not so much in people without Alzheimer’s disease. So a lot more study needs to be done on those there need to be clinical trials, but we see this as a promising approach. And why would that be so important? If you could do the blood tests and you knew before somebody had symptoms, or even very, very early in the course of the disease, the chances of a new drug that’s in the trial, the chances of that working are much higher, we believe. So that’s one of the really important things were applying that to other neurodegenerative diseases as well.
Chris Powell 14:55
Diagnostics are incredibly important and very helpful in helping us determine if we have neurodegenerative diseases. But if you are diagnosed with a disease, the first question that’s going to pop in your head is, well, what can be done about this?
Nick Cochran 15:09
There are a couple of approved symptomatic treatments for Alzheimer’s that can plateau individuals for maybe six months or so. And they can delay nursing home placement by about two years. So these are things like Aricept and Namenda. And so these are important and good that we have in the clinic, but they’re not modifying the underlying disease pathology. But still, we’re at the beginning of disease-modifying therapy for diseases like Alzheimer’s, where we haven’t yet reached that point that we’re at with diseases like HIV or many cancers where there are multiple combinatorial treatments that can really impact disease course in a big way. So I think we’re still working towards that ultimate goal for Alzheimer’s.
L-dopa is a really good treatment option for Parkinson’s that can help individuals, depending on how their particular disease course goes, for many years in some cases. It is still a symptomatic treatment. So it’s not doing anything to the underlying death of the brain cells, but it really helps patients a lot in some cases. The other thing that can help a lot is something called Deep Brain Stimulation. So this is actually a surgery that’s done to implant an electrode deep into the brain into a structure that’s affected by Parkinson’s. So Parkinson’s arises because of degeneration of neurons in an area of the brain called the substantia nigra pars compacta. It’s this very specific region of the brain that’s involved in motor function.
Sarah Sharman 16:49
The first symptom that people often have with Parkinson’s is just a subtle tremor in one hand. Although this is a small symptom, by the time this is noticed, there’s often already 70 to 80% of damage to this part of the brain.
Nick Cochran 17:04
What this deep brain stimulation allows to happen is to partially replicate the function of the loss of those neurons and then promote the function of those that still remain to be able to gain some symptomatic benefit.
Chris Powell 17:22
Hey, Sarah, are you interested in going to Colombia?
Sarah Sharman 17:26
Chris, stay on track, we’re talking about neurodegenerative diseases.
Chris Powell 17:30
We are. That’s a very astute observation. But in order to talk about neurodegenerative disease, we need to talk about Colombia because as we were talking with Dr. Cochran, he told us about some collaborations that are happening between the Institute and other researchers in Colombia. And this collaboration is quite fascinating.
Sarah Sharman 17:49
Fascinating is a great word to describe this study, Chris. So, there’s this family in Colombia, and they have a higher than average rate of early-onset Alzheimer’s disease. And by higher than average, I mean, like one in five individuals with the disease. So normally, we’re looking at people getting Alzheimer’s disease when they’re about 70 to 80 years old. However, this family has generation after generation of members getting the disease as early as ages 40 to 50 years old.
Nick Cochran 18:19
The history of this all starts with a physician named Francisco Lopera, who, many years ago, discovered a group of individuals with a very early onset form of Alzheimer’s disease. And this group of patients has been in the news quite a bit. So, it’s the largest founder population of dominant Alzheimer’s disease in the world, meaning that if someone inherits the mutation, they will, with certainty, eventually develop dominant Alzheimer’s disease. Now, one thing that’s happened and the results just came out, and unfortunately, this was a clinical trial that they set up for this population that ended up being negative, but we’re hoping to learn more information about that soon. And it’s perhaps not surprising, and hopefully, we’ll learn some information that will allow for refined approaches for that population. But because of this, they set up this clinical trial for these individuals, and of course, everyone in these families was excited about participating in this and, hopefully, receiving a treatment that may provide them some benefit.
So people from all over Colombia came to enroll in this trial. And, you know, the clinicians there said, this is great, we, of course, want to get you connected with this treatment option. We just have to, you know, check your genetics and make sure that you really have this genetic change that causes this disease because that’s who this particular trial was for. For many of the individuals, they of course, had this known mutation. And then, for some, they did not. And so, of course, the question is, well, you know that this individual still has early-onset dementia, but they don’t have this one mutation that’s in this large founder population. So, what’s going on with this family? So what came to fruition just in the past few months, we collected samples from these individuals that were not from this large founder family, but still had an early onset dementia, and described the underlying genetics in those individuals.
In addition to these rare patient populations, we’re now also deeply thinking about, along with many others across the country, that we need to right size our patient population genetic cohorts for representation of global ancestries around the world. And so our contribution in this space is to try and help facilitate those efforts across South America. We’re working with 10 different centers across six different countries. So, Colombia, like I mentioned, also, Brazil, Chile, Argentina, Mexico, and Peru. And so, through those efforts, we’ll capture things that may be unique to these ancestral populations, we’ll find things that are shared across the world, and also increase representation for these early onset and rare neurodegenerative diseases. So that’s, that’s ongoing now. It’s really exciting. We’ve already measured genetic data for a couple of 1000 participants. And we’ll continue that that’s it’s had a little bit of a setback with the COVID pandemic, of course, where it’s been difficult for patients to enroll. But despite that, we’ve still been able to do quite a bit. So I’m excited about where that project goes over the coming years.
Chris Powell 22:28
Neurodegenerative disease is something that none of us want to deal with. The thought of losing our memory or motor function or watching someone we love lose those capacities is frightening. The good news is that there are some really amazing scientists working to understand, diagnose, and ultimately treat these diseases. The fight against them is going to be long, but it’s far from over.
Sarah Sharman 22:51
Thank you for joining us for this tiny expedition into the science of neurodegenerative disease. Next time, it’s back to bioethics. We will tackle big picture issues surrounding access to participation in genetic research.
Chris Powell 23:04
We’ll ask questions like, does genetic research and genetic testing benefit everyone equally? And how can we rebuild trust with groups of people who have been mistreated by the medical and research communities?
Sarah Sharman 23:17
Tiny Expeditions is a podcast about genetics, DNA, and inheritance from the HudsonAlpha Institute for Biotechnology. We’re a nonprofit research institution in Huntsville, Alabama.
Chris Powell 23:27
We’ve got a campus full of scientists doing public research alongside companies developing products and services, all with one aim to translate genomic discoveries into real-world applications that make for a healthier, more sustainable world. That’s everything from cancer research to agriculture for changing climate.
Sarah Sharman 23:45
If you find this podcast interesting, rate, review, like, and subscribe on the podcast app of your choice. And tell someone that you listen to this interesting little story about genetics. Knowledge is better when you share it.
Chris Powell 23:57
Thanks again to our sponsor, EBSCO Information Services. And thanks to you, our listeners for joining us.
Season 3 of Tiny Expeditions is made possible through the support of our sponsors: